Pericardial Effusion: Diagnosis And Treatment
The simplest method for diagnosing pericardial effusion is echocardiography. Find out more about this topic today.
A pericardial effusion is a relatively common medical problem. Sometimes there is a connection to a pre-existing illness. In other cases, a specific examination and diagnosis is needed to find out the exact cause. However, it is not always possible to find a specific trigger.
In some cases, pericardial effusion can remain unchanged for years and thus become a chronic disease without haemodynamic consequences.
The aim of the treatment is to solve the underlying problem that leads to pericardial effusion. In addition , it is of course also about treating the symptoms. But when the exact cause cannot be determined, the same clinical treatment as for pericarditis is used.
What is a pericardial effusion?

Pericardial effusion is a pathological accumulation of fluid in the pericardium. This is made up of two layers of connective tissue: Pericardium fibrosum (the outer layer) and Pericardium serosum (the inner layer).
The gap between these two layers, which is also called the pericardial cavity, is filled with fluid (about 10-12 ml). However, when there is inflammation, fluid production increases, which leads to pericardial effusion.
This can also arise, for example, if the absorption of the liquid is too low. This can occur due to the increase in systemic venous pressure. The excessive pressure is often caused by congestive heart failure or pulmonary hypertension.
Pericardial effusion: diagnosis
The clinical impact of pericardial effusion depends on the rate at which the pericardial cavity fills with fluid. Typical symptoms are difficulty breathing and chest pain. Nausea, dysphagia (difficulty swallowing), hoarseness, and hiccups are also common signs.
If a pericardial effusion is suspected, the following tests are usually carried out (usually one or two of them are sufficient):
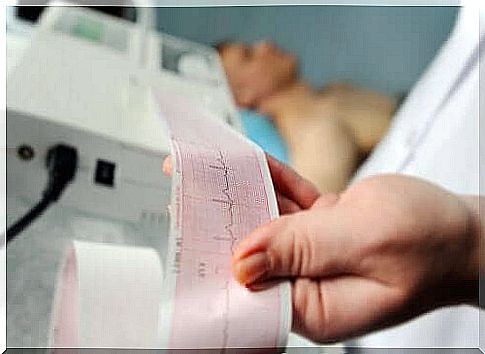
- Echocardiography: This allows the extent of the effusion and the state of the heart function to be recognized. Transesophageal echocardiography provides more detailed images and is therefore more reliable than transthoracic echocardiography.
- Electrocardiogram (EKG): This shows patterns that may indicate cardiac tamponade.
- Thoracic X-ray: This imaging technique allows one to see the global extent of the pericardial effusion.
While echocardiography is the most common diagnostic tool, computed tomography and magnetic resonance imaging provide a wider field of view. However, because these imaging modalities are not always available and are more expensive, they are rarely used to diagnose pericardial effusion.
Echocardiography makes it possible to determine five basic variables: size, time of development, distribution, composition and hemodynamic effects. The next clinical challenge is to find out the exact causes of the problem and initiate the correct treatment.
Pericardial effusion: treatment

Treatment depends directly on the causes of the pericardial effusion. It also plays a role whether or not a pericardial tamponade is present and where the origin of this anomaly lies. Proper treatment can solve the problem.
First, the size of the pericardial effusion and its hemodynamic importance must be assessed. It is also important to identify related diseases. In around 60% of the cases this problem is caused by another disease.
If there is no pericardial tamponade and no risk of it , the doctor usually recommends bed rest and an anti-inflammatory drug. Colchicine and corticosteroids are also commonly used.
If there is any risk of tamponade or the progression of the effusion, a pericardiocentesis or pericardial puncture is usually done to remove the fluid. If this is not possible or unsuccessful, open surgical drainage is necessary. In this case, a biopsy must be performed. A pericardial window is also necessary.
Pericardial effusion: control and prognosis
Idiopathic pericardial effusion and pericarditis generally have a good prognosis. The risk of complications is relatively low. In the case of chronic idiopathic pericardial effusion, the probability of pericardial tamponade is around 30 to 35%.
For the other types , the prognosis largely depends on the cause and size of the effusion. If the size exceeds 10 mm, tamponade will develop in a third of cases.
If the pericardial effusion is moderate, echocardiography should be performed every six months. In severe cases, this examination is carried out every three months. If the pericardial effusion is not idiopathic, check- ups will depend on the cause of the underlying disease.